Prostate Cancer
Overview
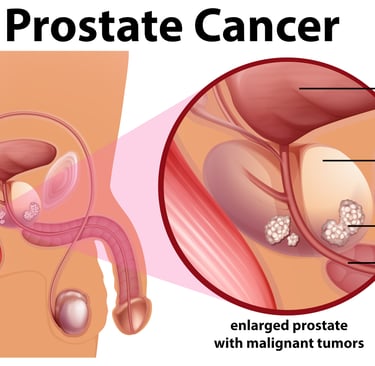
Prostate cancer is one of the most common cancers affecting men, particularly those above 50 years of age. It develops in the prostate gland, a small gland that produces seminal fluid. Most prostate cancers grow slowly, but some can be aggressive and spread rapidly — making early detection vital.
Thanks to advancements in diagnostics and precision treatment, survival rates have significantly improved.
Causes and Risk Factors
While the exact cause of prostate cancer is not completely understood, certain factors increase the likelihood of developing it:
Age: The strongest risk factor — risk increases sharply after 50 years.
Family History: Men with a father or brother diagnosed with prostate cancer are at higher risk.
Ethnicity: More common in African and Afro-Caribbean men, less in Asian men.
Diet and Lifestyle: High-fat diet, obesity, and sedentary lifestyle contribute to risk.
Environmental Exposure: Certain chemicals, such as those used in metalworking and
agriculture, may increase risk.
Genetic Factors
Some prostate cancers are linked to inherited gene mutations, including:
BRCA1 and BRCA2 mutations (also associated with breast and ovarian cancers).
HOXB13 mutation – linked to early-onset prostate cancer.
DNA repair gene defects (ATM, CHEK2, MSH2, MLH1) – can lead to aggressive disease.
Genetic testing helps identify men at higher risk and guide decisions regarding screening and targeted therapy.
Common Symptoms
Prostate cancer in its early stages may cause no symptoms, which is why routine screening is important. When symptoms do occur, they may include:
Difficulty or pain while urinating.
Weak or interrupted urine flow.
Increased frequency of urination, especially at night.
Blood in urine or semen.
Pain in the lower back, hips, or pelvis (in advanced cases).
PSA
Prostate-Specific Antigen (PSA) plays a crucial role in the detection, monitoring, and management of prostate cancer. PSA is a protein produced by both normal and malignant prostate cells, and its level can be measured through a simple blood test. Elevated PSA levels may indicate the presence of prostate cancer, though they can also rise due to benign conditions such as prostatitis or benign prostatic hyperplasia (BPH). PSA testing is used as a screening tool to detect prostate cancer at an early, potentially curable stage, and is also vital for monitoring treatment response and detecting recurrence after surgery or radiotherapy. A rising PSA after definitive treatment often signals biochemical recurrence, prompting further evaluation or salvage therapy. However, interpreting PSA levels requires careful consideration of age, prostate size, and prior treatments to avoid overdiagnosis and unnecessary interventions.
The significance of PSA (Prostate-Specific Antigen) levels depends on the patient’s age, prostate size, and clinical context. Here’s a concise summary of how PSA values are typically interpreted:
Normal PSA Levels by Age:
Age Group Upper Limit of Normal PSA 40–49 years≤ 2.5 ng/mL; 50–59 years≤ 3.5 ng/mL; 60–69 years≤ 4.5 ng/mL; 70–79 years≤ 6.5 ng/mL.
Clinical Significance of PSA Levels
PSA < 4 ng/mL: Generally considered within normal limits, though prostate cancer can still occur, especially in younger men or those with high-risk genetics (e.g., BRCA mutation).
PSA 4–10 ng/mL (Borderline Zone): About 25% risk of prostate cancer. Further evaluation with free/total PSA ratio, PSA density, PSA velocity, or MRI is recommended before biopsy.
PSA > 10 ng/mL: High likelihood (over 50%) of prostate cancer; biopsy is usually warranted.
PSA > 20 ng/mL: Strongly suggests clinically significant or advanced prostate cancer and may indicate extra-prostatic disease.
What is Hormonal Therapy?
Hormonal therapy (Androgen Deprivation Therapy, ADT) is a cornerstone in prostate cancer treatment.
Prostate cancer cells depend on male hormones (androgens) such as testosterone to grow.
Hormonal therapy works by:
Reducing testosterone production using medications like LHRH agonists/antagonists, or
Blocking androgen action using anti-androgen drugs.
It is used in:
Advanced or metastatic prostate cancer.
Before (neoadjuvant) or after (adjuvant) radiation therapy to enhance its effectiveness.
Modern ADT can delay progression, shrink tumors, and improve survival when combined with radiotherapy.
Treatment Approaches
Treatment depends on the stage and aggressiveness of the disease:
Active Surveillance: For slow-growing, localized tumors in elderly or low-risk patients.
Surgery (Radical Prostatectomy): Removes the prostate gland; curative in early disease.
Radiation Therapy: A non-invasive, effective option using precisely targeted radiation beams.
Hormonal Therapy: As mentioned, controls disease progression by reducing testosterone activity.
Chemotherapy or Targeted Therapy: For resistant or advanced cases.
Immunotherapy: An emerging option for select genetic subtypes.
Cutting-Edge Cancer Care by Dr. Rajesh Natte
Dr. Rajesh Natte, a distinguished radiation oncologist, is redefining prostate cancer treatment through advanced precision radiotherapy.
Using Image-Guided Radiotherapy (IGRT), Volumetric Modulated Arc Therapy (VMAT), and Stereotactic Body Radiotherapy (SBRT), he ensures that radiation precisely targets the prostate while sparing nearby organs such as the bladder and rectum.
Through fiducial marker tracking, real-time image guidance, and AI-assisted adaptive planning, Dr. Natte tailors each treatment to the patient’s anatomy and tumor motion — delivering exceptional accuracy and minimal side effects.
This results in shorter treatment duration, better tumor control, and improved quality of life for patients.
Summary
Prostate cancer, though common, is highly curable when detected early and treated appropriately. With advances in hormonal therapy and precision radiotherapy, outcomes have never been better.
Under the expert care of Dr. Rajesh Natte, patients benefit from cutting-edge technology, evidence-based treatment, and compassionate care — bringing together science and empathy to fight prostate cancer effectively.