Cervix Cancer
Overview
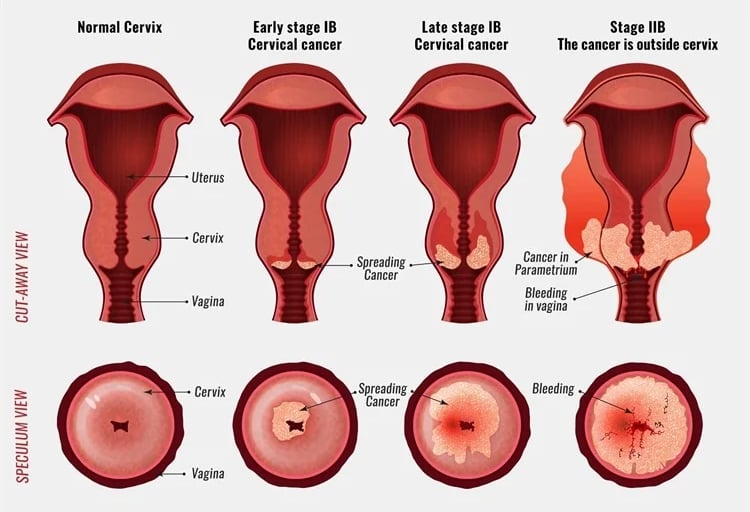
Cervical cancer arises from the lower part of the uterus called the cervix, which connects the uterus to the vagina. It remains one of the most common cancers affecting women in India, yet it is largely preventable and highly curable when detected early. With the advent of HPV vaccination, regular screening, and precision radiotherapy, the burden of cervical cancer is steadily declining.
Causes and Risk Factors
The Human Papillomavirus (HPV) is the primary cause of cervical cancer. Persistent infection with high-risk HPV types — particularly HPV 16 and 18 — leads to precancerous changes in cervical cells that may progress to cancer if untreated.
Other risk factors include:
Early onset of sexual activity and multiple sexual partners.
Long-term use of oral contraceptives.
Smoking.
Weakened immune system (HIV infection).
Poor genital hygiene and lack of screening.
Common Symptoms
Early cervical cancer is often asymptomatic, which underscores the importance of regular screening. As the disease progresses, common symptoms include:
Abnormal vaginal bleeding — after intercourse, between periods, or after menopause.
Foul-smelling or watery vaginal discharge.
Pelvic pain or pain during intercourse.
Backache or leg swelling in advanced stages due to tumor spread.
Any of these persistent symptoms should prompt medical evaluation.
Screening and Prevention
Cervical cancer is one of the few cancers that can be prevented through vaccination and screening.
Key preventive measures include:
HPV Vaccination: Recommended for girls and women between ages 9–26, ideally before the onset of sexual activity. The vaccine protects against high-risk HPV strains that cause most cervical cancers.
Regular Screening:
Pap Smear Test: Detects precancerous changes; should begin at age 21 and continue every 3 years.
HPV DNA Test: Identifies infection by high-risk HPV types; can be done every 5 years (alone or combined with Pap test).
Safe sexual practices and smoking cessation further reduce risk.
Early detection through screening can prevent up to 90% of cervical cancers.
Treatment Approaches
Treatment depends on the stage of disease, age, and reproductive goals. The main modalities include:
Surgery: For early-stage cancers, procedures such as conization, hysterectomy, or radical trachelectomy (fertility-sparing surgery) may be performed.
Radiation Therapy: Plays a central role in locally advanced disease, often combined with chemotherapy (concurrent chemoradiation).
Chemotherapy: Used as a radiosensitizer or in recurrent/metastatic disease.
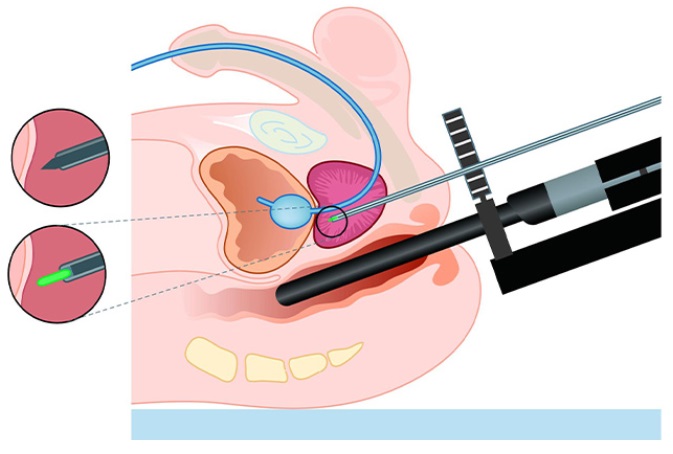
Brachytherapy (Internal Radiation):
A crucial part of curative treatment for cervical cancer.
Intracavitary brachytherapy is used for most patients, while interstitial brachytherapy is used when the tumor extends beyond the cervix or when anatomy is distorted.
Interstitial brachytherapy involves placing radiation sources directly into the tumor using needles, ensuring precise dose delivery to cancerous tissue while sparing the bladder and rectum.
Cutting-Edge Cancer Care by Dr. Rajesh Natte
Dr. Rajesh Natte, a leading radiation oncologist, is transforming the treatment of cervical cancers with advanced image-guided and adaptive radiation techniques.
By integrating Image-Guided Radiotherapy (IGRT), Intensity-Modulated Radiotherapy (IMRT), and Volumetric Modulated Arc Therapy (VMAT), he ensures high-precision targeting of tumors with minimal damage to surrounding healthy tissues.
In cervical cancer care, Dr. Natte’s expertise in MRI-based image-guided brachytherapy (IGBT) and interstitial techniques allows for unparalleled precision — improving local control, reducing complications, and preserving organ function. His use of AI-assisted planning and real-time dose optimization brings world-class quality and accuracy to every patient’s treatment journey.
Summary
Cervical cancer is both preventable and curable when detected early and treated effectively. With widespread vaccination, regular screening, and access to cutting-edge radiotherapy, its impact can be drastically reduced. Under the care of Dr. Rajesh Natte, patients benefit from state-of-the-art technology, evidence-based protocols, and compassionate, personalized care — setting new standards in the fight against gynecological cancers.